During Grand Morning Report, we briefly discussed a patient
with sickle cell disease and a history of acute chest syndrome. This is a common complication of sickle cell disease and is a frequent cause
of death in this patient population, making early diagnosis and treatment critical.
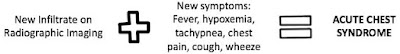
What is acute chest
syndrome?
What causes acute
chest syndrome?
A number of different causes for acute chest syndrome have been
identified. These include the following:
- Pulmonary infarction due to vaso-occlusion from sickled cells
- Fat embolism due to release of fat into the bloodstream from bone marrow infarction during a vaso-occlusive crisis
- Infection
- Hypoventilation
It is also important to recognize that patients can present
with what appears to be a straightforward pain crisis and still go on to
develop acute chest syndrome during their hospitalization.
What else should be
on the differential?
Given that many of the features of acute chest syndrome are
vague or non-specific, other etiologies for the patient’s presentation should
be considered and/or ruled out. The
following are alternate diagnoses not to miss:
- Acute coronary syndrome
- Pulmonary embolism
- Exacerbation of asthma or COPD
- Pneumonia (although this is often indistinguishable from acute chest syndrome)
How is acute chest
syndrome treated?
The mainstays of treatment for a vaso-occlusive crisis still
apply:
- Early and aggressive pain control
- IV fluids to maintain normovolemia
- Oxygen
- Incentive spirometry
- DVT prophylaxis
However, the following therapies should also be considered, along with Hematology consultation:
Antibiotics:
- Since it is often impossible to distinguish pneumonia from acute chest syndrome, patients should be started on antibiotic therapy early. This should also include coverage for atypical organisms as mycoplasma pneumoniae and chlamydia spp. are thought to be frequent culprit organisms.
·
Simple vs. Exchange Transfusion:
- Simple transfusion should be considered for mild acute chest syndrome while patients with moderate to severe disease typically require exchange transfusion. The goal of both therapies is to lower the overall proportion of hemoglobin S and improve oxygenation.
References and more reading...
Paul RN, et
al. “Acute chest syndrome: sickle cell
disease”. Eur J Haematol. 2011 Sep;87(3):191-207.
Vichinsky EP, et al.
“Causes and outcomes of the acute chest syndrome in sickle cell
disease. National Acute Chest Syndrome
Group”. NEJM; 2000 Jun
22;342(25):1855-65.