Acute asthma exacerbations are relatively common internal medicine referrals. Some points on managing this potentially life-threatening condition:
Indicators of severity:
Clinical- SILENT CHEST, pulsus paradoxus, acc muscle use, diaphoresis, inability to speak
Peak flow- less than 200 or less than 50% of baseline is severe attack
ABG- hypoxia is rare, and indicates very severe. Hypercapnia or even normal PCO2 is bad; indicates tiring.
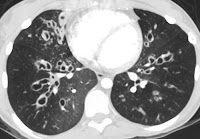
CXR- unhelpful usually; may do to exclude pneumothorax (possible complication), pneumonia.
Very important to get a peak flow reading on presentation and then monitor closely q1-2h during therapy to assess progress.
Therapy
1) B-agonist: Mainstay of therapy
Salbutamol 4-6 puffs q1-2h iniitally. Outcomes with inhaler vs. nebulizer are essentially equal assuming proper technique. 1 NEB treatment generally equals 4-6 MDI puffs with a spacer.
2) Ipratroprium: Added if not initially responding or if severe.
Especially recommended for pts with COPD or B-Bl triggered asthma.
Ipratroprium 500mcg NEB q6-8h (can be given with 1st ventolin neb treatment) or MDI 2 puffs of 17mcg each q6h.
3) Steroids:
Consider if:
1) less than 10% increase in PF after 1st dose of B-ag
2) attack in pt on oral steroids before attack
3) PF less than 70% predicted after 1h of treatment
Only difference between PO and IV steroids is onset of action; within 1d for IV vs possibly 2d for PO. Otherwise equivalent. Dose of steroid is not clear. For severe, a commonly studied dose is Solumedrol 125mg IV q6h x 3d. For less severe, consider Solumedrol 30mg IV q8h x 3d then switch to oral.
PO: Prednisone 1-2mg/kg/d divided q 8-12h for 2-4d, then reduce. All pts who received steroids should get oral steroids on discharge; usually prednisone on tapering regimen for 8-10d, but also acceptable if steroid naive to keep on prednisone for 1 week, reassess, and d/c abruptly if less than 10d
4) MgSO4: Some evidence of benefit; blocks SM contraction. 2g IV over 20min. Little toxicity to this dose
5) Epinephrine: last resort; patient will probably need intubation.
6) Final step is rapid sequence induction and intubation by the most skilled person available (there may only be 1 chance), and initiation of inhaled anesthetics (which are bronchodilators). Ketamine is also a bronchodilator.
Little or no role for antibiotics, theophylline, montelukast
Consider admission if:
-peak flow less than 40% of predicted after bronchodilators or less than 25% on arrival
-any hypoxia, distress, etc.
Consider ICU or intubation if:
-Clinically tiring or in respiratory distress
-Hypercapnea or hypoxia
-Worsening on therapy
-PF less than 150
Links:
Click here for acute exacerbation guidelines from 2007
Click here for evidence for magnesium in acute exacerbation