The easiest way to approach this clinical problem is to think about the various infections that can infect patient as the CD4 count declines, and their overall risk for infections increases. It is step-wise, and so obviously if your CD4 count is less than 100 you are at risk for all of the illnesses at the preceding steps (i.e. if CD4 count < 100 you are at risk for Toxoplasmosis, Cryptococcus and PCP, thrush, and TB).
 |
| Courtesy of Wikipedia - HIV virus (green) and a lymphocyte |
In any patient with HIV, irregardless of the CD4 count, Mycobacterium Tuberculosis (TB) can cause both pulmonary, and extra-pulmonary infections. The current recommendations from the CDC are that any patient with HIV be screened for latent TB with a TB-skin test. If a patient screens positive, and they have no evidence of active TB (i.e. pulmonary TB) then they should be treated for latent TB for 9 months (CDC guidelines).
Other infections to consider irregardless of the CD4 count include both bacterial and viral infections:
Streptococcus pneumoniae, influenza A/B, Human Papillomavirus (HPV), VZV, and Hepatitis A/B.
Fortunately, all of these pathogens have appropriate vaccines, and so making sure your patient has up to date vaccinations is a critical step.
Vaccinations:
1. Streptococcus pneumoniae (13-valent or 23-valent vaccine) - check guidelines for further details
2. Influenza A/B - seasonal vaccine each year
3. VZV - Varivax if never received it / or never exposed
4. HPV - for both male and females (13-26 years of age) - quadrivalent HPV vaccine
5. Hepatitis A/B - Hep A vaccine, Hep B vaccine, and combined Hep A/B vaccine
CD4 count < 250 - Coccidiodomycosis
If you reside in an endemic area for coccidiodomycosis (beautiful Arizona or California) then prophylaxis with fluconazole 400 mg PO daily should be initiated.CD4 count < 200 - Pneumocystis Pneumonia (PCP) and Thrush (esophageal candidiasis)
Any patient with a CD4 count less than 200 or oral thrush/history of an AIDS defining illness should receive prophylaxis for PCP. This is usually in the form of Septra (TMP-SMX). Alternatives include Dapsone and aerosolized pentamidine.The CDC does not recommend routine prophylaxis against esophageal candidiasis because it is highly treatable with fluconazole, and does not have a high associated mortality.
CD4 count < 150 - Histoplasmosis
Similar to coccidiomycosis, if you reside in an endemic area and the patient is at high risk because of occupational exposure or the location is a hyperendemic area, then prophylaxis with Itraconazole can be considered.CD4 count < 100 - Toxoplasma Gondii and Cryptococcus
When the CD4 count drops below 100 your patient is at risk for developing both Toxoplasma and Cryptococcus. Toxoplasma can cause space occupying lesions, seizures and other severe neurological symptoms. Cryptococcus can present as insidiously and ultimately lead to a meningitis.Prophylaxis for toxoplasma consists of Septra, and so if your patient has a CD4 count less than 100 they are most likely already going to be receiving Septra for PJP prophylaxis. No prophylaxis is currently indicated for cryptococcus.
CD4 count < 50 - Mycobacterium Avium Complex (MAC) disease
If the CD4 count has drifted to below 50, then your patient is at risk for all of the above opportunistic infections and MAC. The prophylaxis for MAC infection is a macrolide antibiotic (Azithromycin 1200 mg PO once weekly) or Clarithromycin. before initiating prophylaxis, the clinican should first rule out active disease.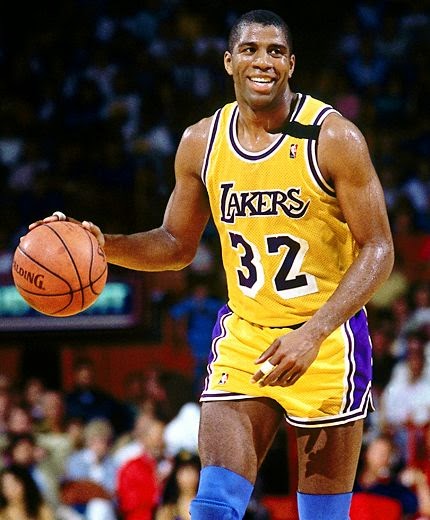 |
| Magic - Many people still remember his November 7, 1991 press conference when he announced to the world that he was HIV positive. Times have changed greatly since then! |
Conclusions:
The most important management decision when looking after a patient with HIV is the initiation of HAART (Highly Active Antiretroviral Therapy). HAART has been one of the most incredible advances in medicine over the past few decades. Many patients are able to maintain a normal CD4 count with undetectable viral loads for many years, and do not develop any of these opportunistic infections.As Dr. HPK noted, in the 1980's the Toronto Western Hospital had dozens of patients admitted at any one time with pneumocystis pneumonia or cryptococcal meningitis. Today, it is increasingly rare for internists to manage these problems.
Reference:
CDC Guidelines on opportunistic infections
http://aidsinfo.nih.gov/guidelines/html/4/adult-and-adolescent-oi-prevention-and-treatment-guidelines/392/whats-new